Introduction
Agricultural poisons generally includes Pesticides. Pesticides are the compounds used to kill pests. Pests may include insect, rodent, fungi etc. Pesticides are classified as:
- Insecticides: these are the compounds used to kill or repel insects and related species. Examples are — organophosphates, carbamate, organochlorine, pyrethroids.
- Rodenticide: these are the compound used to kill rodent like rat, mice, mole etc. Examples are — zinc phosphide, barium carbonate, strychnine, warfarin etc.
- Herbicide: these are the compounds used to kill weed. Examples are — acrolein, glyphosate, paraquat etc.
- Fungicide: these are the compounds used to kill fungi and moulds. Examples are — thiocarbamate, sodium azide.
- Miscellaneous compounds include lead, copper, mercury, nicotine etc.
Organophosphorus compounds
- Organophosphate poisoning is the most common poisoning in India followed by aluminium phosphide. Organophosphorus compounds are available as dust powder or liquid.
- Organophosphorus compounds are classified as:
- Alkyl compounds — such as tetraethyl pyrophosphate (TEPP), hexa ethyl tetraphosphate (HETP), octa methyl pyrophosphate (OMPA), malathion etc.
- Aryl compounds — such as parathion, chlorothion, diazinon (Tik-20), paraoxon etc.
Absorption, metabolism and excretion
- Organophosphorus compounds are absorbed by any route— skin, conjunctiva, inhalation, oral or by direct injection.
- Some compounds such as parathion are stored in body fat and are released slowly in the circulation thus prolonging the duration of toxic action
- Parathion is first metabolized to paraoxon, which is the active toxic agent and then to paranitrophenol that is excreted into urine.
- Malathion is metabolized in liver by esterases and part of this metabolized product is excreted in urine as phosphate.
Mechanism of action
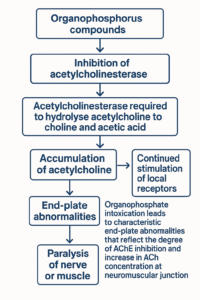
- Organophosphorus compounds are inhibitors of acetylcholinesterase.
- Acetyl cholinesterase is required to hydrolyse acetylcholine to choline and acetic acid .
- As a result, there is accumulation of acetylcholine with continued stimulation of local receptors and eventual paralysis of nerve or muscle.
- Organophosphate intoxication leads to characteristic end-plate abnormalities that reflect the degree of AchE inhibition and increase in Ach concentration at the neuromuscular junction.
Fatal Dose
- Malathion about 1 gm orally
- TEPP Tetraethyl pyrophosphate 45-50 mg IM or IV 100 mg orally
- OMPA Octa methyl pyrophosphate 80 mg by IM or IV 175 mg orally
- Parathion 80mg by IV or IM and 175 mg orally
- HETP Hexa ethyl tetraphosphate 160 mg by IV or IM; 350 mg orally
- Diazinon 1 gm orally
Fatal period:
- Fatal doses: death in half to three hours or few more hours
- In acute effects: non fatal dose: 48 to 72 hours or 3 weeks
Clinical Features
Organophosphate insecticide poisoning in human can produce:
- Acute poisoning: due to acute peripheral and central cholinergic block
- An intermediate syndrome with weakness
- A delayed distal polyneuropathy
Acute Poisoning
- Muscarinic effects: Due to muscarinic like action, following clinical features are observed
- Bronchial tree — cough, increased secretions, bronchoconstriction, wheezing, dyspnea, pulmonary edema.
- Gastrointestinal — nausea, vomiting, abdominal cramp, diarrhea.
- Sweat glands — increased sweating.
- Salivary glands — increased salivation. Mnemonic: “DUMBELS”: Diarrhoea, Urination, Miosis, Bronchospasm, bradycardia, Emesis, Lacrimation, Salivation
- Lacrimal glands — increased lacrimation. Chromodacryorrhea (shedding of red tears) due to accumulation of porphyrin in the lachrymal glands is seen very rarely.
- Eyes — miosis, blurring of vision or dimness of vision. Miosis develops due to the inhibition of cholinesterase and marked parasympathomimetic stimulation of iris. However, dilatation of pupil in organophosphate intoxication have been recorded, therefore, it is essential not to rely only on pupillary size as diagnostic criteria for organophosphate compound poisoning.
- Heart — slow pulse, hypotension.
- Urinary bladder — frequency of micturation increases and there is urinary incontinence.
- Nicotinic Effects:
The nicotinic effects are as follows:
- Striated muscles: easy fatigue, weakness, muscular twitching, fasciculation, cramps
- Sympathetic ganglia: pallor, occasional elevation of blood pressure (hypertension), tachycardia
- Increased adrenal medulla activity
Mnemonic: “MATCH”
Muscle weakness, Adrenal medulla activity, Tachycardia, Cramps in muscles, Hypertension
CNS effects
Irritability
Apprehension
Restlessness
Fine fibrillary tremors of hands, eyelids, face or tongue
Muscular weakness
- Convulsions — the convulsions may be tonic (limbs stretched and rigid) or may be clonic (rapid repetitive movement). Clonic convulsions are more common.
- Mental confusion progressing to stupor to coma
- Depression of respiratory and circulatory centers
Causes of death
- Respiratory failure
- Cerebral hypoxia
- Hyperthermia
- Hepatic failure
- Renal failure
Intermediate syndrome
- Intermediate syndrome is a neurotoxic effect that appears after acute cholinergic crisis but before the expected onset of delayed neuropathy.
- The cardinal feature of the syndrome is muscular weakness, affecting predominantly the proximal limb muscles and the neck flexors. Cranial nerve palsies are common. (The intermediate syndrome predominantly affect muscles innervated by the cranial nerves — neck flexors, proximal muscles of the limb and the muscles of respiration).
- This syndrome carries a risk of death because of the associated respiratory depression.
- The muscle weakness has an acute onset, noticed within 24 to 96 hours after poisoning.
Delayed polyneuropathy:
- Delayed polyneuropathy appears 2 to 3 weeks after poisoning.
- The delayed polyneuropathy is due to inhibition of enzyme neurotoxic esterase with nerve demyelination.
- In delayed polyneuropathy, the paralysis is usually limited to the distal muscles of the limbs; cranial nerves and respiratory muscles are spared.
- The disorder is characterized by flaccid weakness and atrophy of distal limb muscles or spasticity and ataxia.
Diagnosis:
- Cholinesterase levels
- Depression of RBC cholinesterase level more than 50 percent of normal indicates organophosphate poisoning.
- The decrease is due to binding by phosphate group of pesticide. It is better parameter than plasma cholinesterase.
- Depression of plasma (serum) cholinesterase activity more than 50 percent of normal indicates Organophosphate poisoning. This test is not specific as plasma cholinesterase activity is also depressed in cirrhosis of liver, neoplasia, malnutrition, septicemia due to burns, obstructive jaundice.
- Colorimetric method
- 1 ml sample urine is taken and 1 ml of NBB(Napthol Blue Black) {45% in acetone 4-(nitrobenzyl) pyridine} added and mixed for 30 seconds in vortex mixer. The mixture is heated at 100o C for 20 minutes. Organophosphate insecticide shows a characteristic purplish blue color that can be read using spectrophotometer.
P-nitrophenol test
Paper chromatography
- Thin layer chromatography (TLC)
- Gas chromatography (GC)
- Gas chromatography-mass spectrometry (GC-MS)
- High performance liquid chromatography (HPLC)
- ECG may show right axis deviation, ST segment depression and T wave inversion
Management
The principles of treatment are as follows:
- Stabilization of patient
- Decontamination
- Antidote administration
- Supportive measures
- Nursing care
Stabilization of the patient: ABC (airway breathing and circulation is checked and restored and the vitals are constantly monitored.
Decontamination:
Skin — the affected part should be washed thoroughly with copious water
Ocular — copious eye irrigation with normal saline or tap water
Ingestion — gastric lavage and administration of activated charcoal.
Antidote administration:
- Atropine is competitive antagonist of acetylcholine and blocks muscarinic manifestations of Organophosphate.
- It does not reverse peripheral muscular paralysis, which is nicotinic action. The atropine should be given 2 mg intravenous promptly with dose repeated every 10 or 15 to 30 minutes till pupil dilates (up to 200 mg has been administered in a day).
- Some authorities recommend administration of atropine until bronchial and other secretions have dried. According to them pupil size and heart rate cannot be used as end-points. Continued treatment with maintenance doses may be required for 1 to 2 weeks
- Oximes are used as they helps to regenerate acetylcholinesterase at muscarinic, nicotinic and CNS sites.
- Pralidoxime (2-PAM) is given intravenously as 500- mg/20 ml (5% isotonic solution) infusion in a dose of 1 to 2 gm (children 20 to 40 mg/kg). Given every 12 hours.
Supportive measures:
- Oxygen administration, ventilator assistance
- Maintain vital parameters, hydration, urine output
- Convulsions should be controlled with judicious use of diazepam
Avoid giving Other acetylcholinesterase inhibitors such as Physostigmine, Endorphonium (competitive AchE inhibitor), Succinylcholine for rapid intubation
Autopsy Findings
- Insecticide like smell (sometimes garlicky or kerosene like)
- Froth at mouth and nostrils
- Cyanosis
- Constricted pupils
- Stomach contents have insecticide like smell. Mucosa stained with compound color, congested and eroded
- Congestion of organs
- Pulmonary edema
- Cerebral edema
- Features of toxic myocarditis had also been reported.
- Microscopic examination of heart reveals dilatation of pericardial blood vessels with hemorrhages in the surrounding tissues,
- Interstitial edema of myocardium, inflammatory cells, hemosiderin-laden macrophages and fatty infiltration of the myocardium.
Medicolegal Importance
- Accidental poisoning may occur in farmers while spraying in the fields or opening the lid of the containers.
- Suicidal poisoning is common with this insecticide.
- Homicidal is rare as it is difficult to mask the smell of insecticide.
- Even though sometimes mixed with alcohol for homicidal purposes


Pyrethrum derivatives
- Pyrethrum is extract of the chrysanthemum flower.
- Pyrethrum contains six active components labeled pyrethrins.
- Pyrethroids are synthetic derivatives of pyrethrins.
- These compounds are commonly used as insect and mosquito repellants.
- Examples — allethrin, D-allethrin, cypermethrin, permethrin etc.
Mechanism of action:
- Pyrethroids prolong the inactivation of the sodium channel by binding to it in the open state.
- These compounds quickly inactivate insects but mammals are relatively resistant to them. However, in most of the cases, toxicity with these agents occurs because of the allergic reactions to these compounds.
Management:
- Decontamination
- Skin — the affected part should be washed thoroughly with copious water
- Ocular — copious eye irrigation with normal saline or tap water.
- Systemic poisoning:
- Ingestion — Gastric lavage and administration of activated charcoal
- Fatty substance should be avoided as they promotes the absorption through GIT
- Allergic reaction should be treated with epinephrine and antihistamine
- Bronchospasm should be treated with appropriate bronchodilators
- Convulsions should be controlled with judicious use of diazepam
- Oxygen administration, ventilator assistance.
Autopsy findings
- Insect repellant like smell
- Froth at mouth and nostrils
- Cyanosis
- Congestion of organs
- Pulmonary edema
- Cerebral edema
Medicolegal importance
- Accidental poisoning may occur.
- Suicidal poisoning is rare
Aluminum Phosphide
- Aluminum phosphide is used as a grain preservative. In northern part of India, it is the leading cause for death due to poisoning.
Availability
- Aluminum phosphide is available in grayish green tablets of 3 gm each.
- Each tablet release 1 gm of phosphine.
- In India: Phosphite and hydrophosphite of aluminum are used for grain preservatives
- The tablets are available in market with various trade names such as — celphos, alphos, sulphas etc.
- Fatal Dose: 1-2 grams or up to 3 grams
- Fatal Period: 1- 4 hours, majority die within 24 hours
Mechanism of Action
- Aluminum phosphide liberates phosphine when it comes in contact with air and moisture.
- It reacts with acidic media(HCL) of stomach and release phosphine gas, which is rapidly absorbed from gastrointestinal tract by simple diffusion.
- Phosphine is a protoplasmic poison interfering with enzymes and protein synthesis.
- It has cytotoxic action
- It acts by inhibiting the electron transport resulting from preferential inhibition of cytochrome oxidase
Clinical features
- Metallic taste
- Vomiting
- Thirst
- Burning sensation
- Pain in abdomen
- Diarrhea
- Persistent hypotension with shock
- Dyspnea
- Cough
Tachycardia
Tachypnea
Bleeding diathesis
Restlessness
Altered sensorium
Coma
Respiratory distress.
Diagnosis
- Garlicky smell
- Altered liver function tests with raised transaminase levels
- Increased PT and PTT
- ABG shows metabolic acidosis
- ECG — sinus tachycardia, ST depression in leads II and III.
- Silver nitrate test – the patient is asked to breathe through a piece of filter paper impregnated with 0.1 N silver nitrate solution for 5 to 10 minutes. If filter paper becomes black, it suggests presence of phosphine. The blackening is imparted because phosphine reduces silver nitrate to silver.
Management
- Secure airway, oxygen, ventilator assistance
- Manage shock with intravenous fluid and inotropic support
- Manage metabolic acidosis with sodium bicarbonate
- Gastric lavage with potassium permanganate and repeated 2-3 times to oxidize the poison (Gastric lavage is contraindicated with water)
- Activated charcoal 100 g orally
- Liquid paraffin: for excretion of ALP
- Magnesium sulfate administration remains controversial.
- It is said that administration of magnesium sulfate is beneficial for management of cardiac arrhythmias
- Low dose dopamine infusion 4-6 micrograms/kg/min is useful
- I.V hydrocortisone 400 mg every 4-6 hours is highly effective
- According to a study in 2018, Boric Acid is a potent antidote in Aluminum Phosphide poisoning.
Autopsy findings
- Typical garlicky odor
- Congested organs
- Bright fluid blood
- Pleural effusion
- Pulmonary edema
- Toxic myocarditis
- Bleeding diathesis
- Gastric mucosa shows shedding
- Kidney shows acute tubular necrosis
- Liver shows fatty change, congestion, edema, inflammatory infiltrate in portal tract and centrizonal necrosis
Medicolegal Importance
- Suicidal poisoning is common with this agent, especially in the northern part of India.
- Rarely accidental poisoning may occur to workers working in grain elevators, ware houses and grain freighter etc.
Organochlorides
- They are also called chlorinated compounds
- These insecticides are synthesized from dichloro propene (DD)
- Common ones are DDT, Endrin, gammexane, Dieldrin
- Endrin poisoning is more common in India
Endrin
- Endrin is most toxic out of all
- It is synthetic, fat-soluble and water-insoluble
- It has unpleasant taste
- It is stable for months or more
- Market names are: Endrin-We 16, Endox-DB-50, Endtox EC-20, Endrex, Tafdrin etc
- These preparations contain endrin in 20-50% concentration with 50-80% solvent (aromax)
- It is used against insects of cotton, paddy, sugarcane and tobacco.
- Known as Plant penicillin.
- Very common in Andhra Pradesh
Signs and symptoms
- Toxic effects starts rapidly after ingestion
- Salivation
- Vomiting
- Abdominal pain
- Tremors
- Convulsions
- Oozing of fine white froth
- Blood stained froth
- Severe dyspnea
- Convulsions-coma-respiratory failure-death
Fatal dose: symptoms appear after 1 gm, lethal dose is 6 gm
Fatal period: half an hour to several hours. Majority die within 1-2 hours
Management
- Largely symptomatic
- Care of airway
- Decontamination
- Barbiturates and diazepam for convulsions
- Calcium decreases toxicity of endrin (dose: 10 ml of 10% solution I.V every 4-6 hours
- If convulsions are controlled, recovery is likely
Postmortem appearances
- Changes are suggestive of asphyxia
- Externally kerosene like smell from mouth and nostrils
- Fine white froth sometimes blood stained
- Face and finger nails cyanosed
- Injected conjunctiva
- Pupils dilated
- Respiratory passages contain frothy mucous
- Mucus membrane congested
- Petichial hemorrhage in lungs and heart
- Lungs are large and bulky with pulmonary edema
- Blood is dark and fluidic
- Mucus membrane of esophagus, stomach and intestine are congested
- Kerosene like smell from the contents
- Liver, kidney and brain are congested
- It resists putrefaction
- Viscera are preserved in saturated saline
Medicolegal Aspects
- It is freely available and cheap
- Mostly used for suicidal purposes despite unpleasant taste and painful death
- May be used for homicidal purpose by mixing with alcohol
- It can be mixed with sweets
- The toxic dose is small
- Before recognition, damage is already done
- Accidental deaths may occur by use as insecticide
